The U.S. Food and Drug Administration applied its most serious warning label for medical devices to breast implants on October 27, 2021.
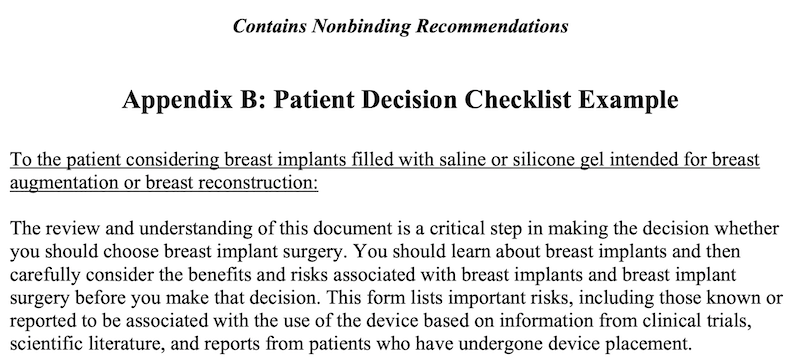
Breast implant manufacturers are now required to supplement their labelling to include a boxed warning about health problems that may arise from the products, and to provide a patient decision checklist that advises of the risks and possible side effects of breast implants.
“Breast implants have been associated with systemic symptoms.”
U.S. FDA
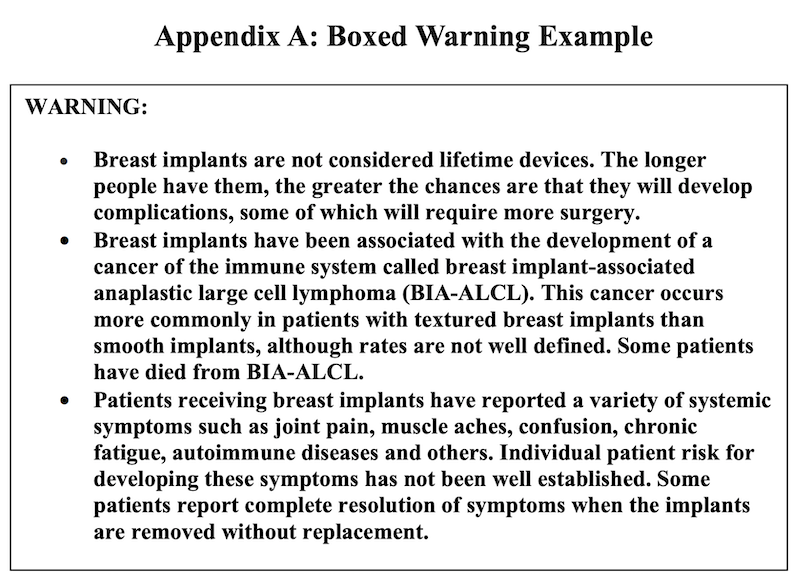
Considered the agency’s most stringent warning, the black box warning informs patients that implants will not last a lifetime. The purpose is to ensure patients understand that the products have been associated with the development of cancer of the immune system.
The FDA says its boxed warning is “commonly referred to as a ‘black box warning.’” and is “designed to call attention to serious or life-threatening risks.”
This warning from the FDA is a response to findings from a March 2019 FDA General and Plastic Surgery Devices Advisory Panel. During the hearing, women shared their struggles with cancer and a variety of debilitating conditions, including brain fog, fatigue, rash and muscle or joint pain that developed after implant surgery. These conditions are often referred to as “breast implant illness.”
Women who had implants placed also stated that they were not adequately warned of the potential health complications of breast implants, nor were they told that implants were not lifetime devices. As a result, the FDA said it has decided to restrict the sale of the products only to health care providers who offer patients a standardized checklist that explains the risks.
Breast augmentation is among the top five most commonly performed cosmetic procedures in the United States as doctors perform about 400,000 surgeries using the implants each year–300,000 for cosmetic reasons and 100,000 for breast reconstruction after mastectomies.
Guidance details
According to the guidance titled “Breast Implants—Certain Labeling Recommendations to Improve Patient Communication,” the boxed warning should clearly state that breast implants can cause a type of cancer of the immune system called BIA-ALCL and that people with silicone or saline breast implants have developed this rare disease, which can be deadly. The warning must also add that the associated risks increase over time as the longer people have them, the greater the chance they will develop complications, some of which may require additional surgery.
“The new requirements follow years of complaints from tens of thousands of women who received breast implants and later suffered from brain fog, fatigue and other health issues, collectively known as “breast implant illness.”
Washington Post, October 27, 2021
Going further, the guidance advises that patients should receive a decision checklist and information brochure highlighting situations in which the device should not be used, the risks associated with BIA-ALCL and surgery, and a discussion of options other than breast implants. The risks in the checklist are in addition to common surgical risks such as infection, necrosis (skin death), or problems with anaesthesia. Patients are expected to sign the checklist to confirm their understanding and agreement with the information.
Additionally, the guidance by the FDA for the first time requires makers of implants to disclose ingredients used to manufacture their products. The agency also suggests rupture screening recommendations, including that screening should begin between five and six years after surgery and then a repeat every two or three years.
Expatiating on the labelling recommendations, the administration further stated in a press release that the labeling recommendations are meant to enhance, but not replace, discussions between doctors and patients.
Ongoing issues
The new requirements have generated mixed reactions in the medical community as some believe it necessary to inform patients of the potential risks and side effects of the procedure. In contrast, others believe the requirements will be ineffective since plastic surgeons are usually eager to reassure their patients, which increases the likelihood that the new checklist will be presented as something unworthy of consideration.
While the New York Times agreed that the guidance provided by the FDA may yield some positive results, the paper also expresses concerns that it is not clear how new requirements will be enforced, especially since “patients are highly unlikely to ever see a warning label on a packaged sterile medical device that is usually handled only by a surgeon.” The newspaper also adds that critics say the checklist is “overly long and written in obtuse language.”
Speaking to the Washington Post, Dr. Scot Glasberg, who sits on the executive committee of the American Society of Plastic Surgeons, believes the new requirements may benefit doctors because they can help decrease their liability risk.
“Surgeons have a liability risk, and this helps to decrease their liability risk… That’s good for patients, and that’s good for surgeons,” says Dr. Glasberg. “I actually believe this is good for everyone.”